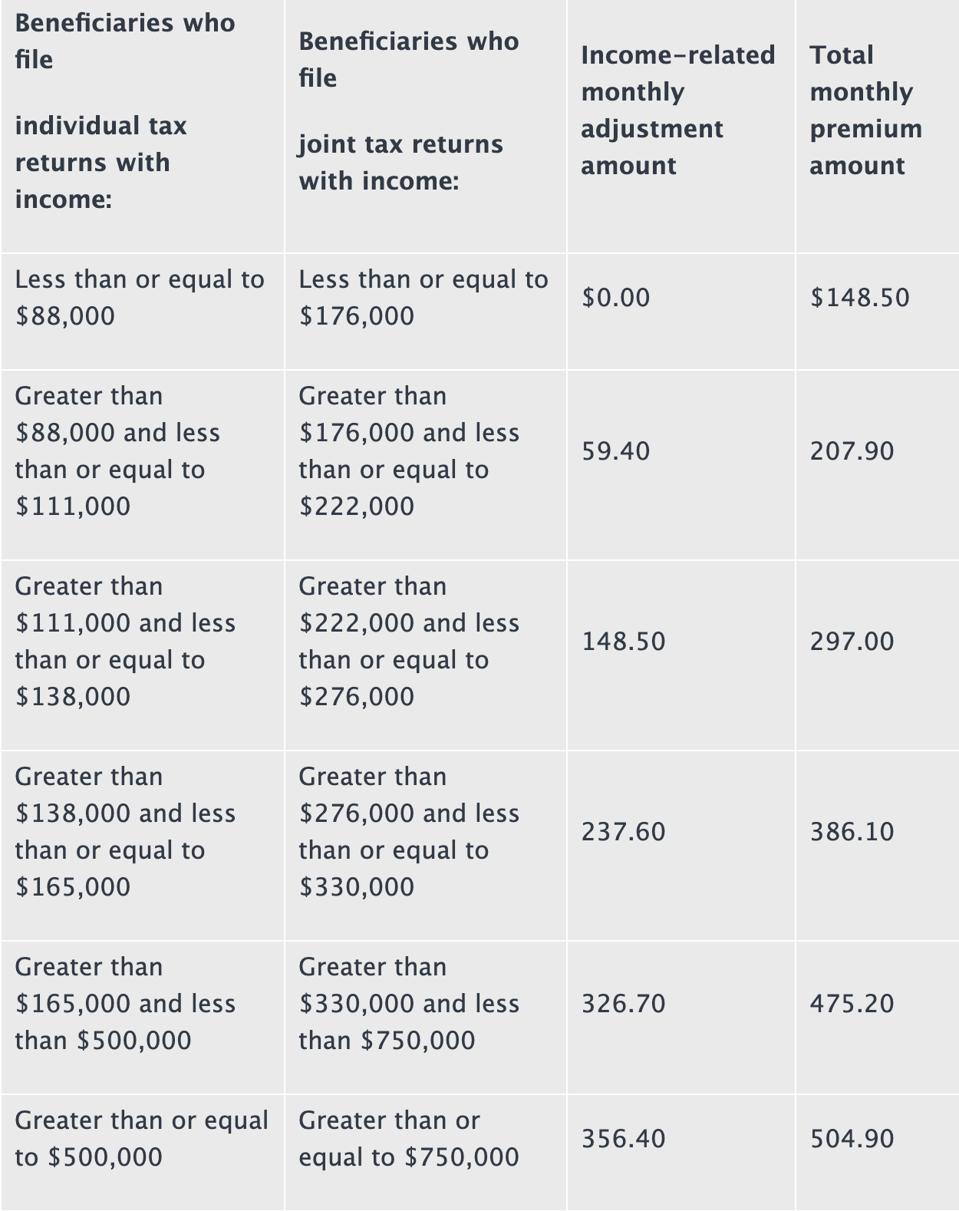
Providing 2022 Medicare Part D Program Compared to 2021, 2020, 2019, 2018, 2017, 2016, 2015, 2014, 2013, 2012, 2011, 2010, 2009, 2008, 2007 and 2006 Also, detailed information on the Medicare Part D program for every state, including selected Medicare Part D plan features and costs organized by State. Sign-up for our free Medicare Part D Newsletter, Use the Online Calculators, FAQs or contact. In general, Part A covers: Inpatient care in a hospital. Skilled nursing facility care. Nursing home care (inpatient care in a skilled nursing facility that’s not custodial or long-term care) Hospice care. Home health care. 2 ways to find out if Medicare covers what you need. Talk to your doctor or other health care provider about why you. Beneficiaries who have Original Medicare and who receive outpatient care must pay the 2020 Part B deductible of $198 per year before Medicare covers the costs of their outpatient care. After meeting the Part B deductible, beneficiaries typically pay a 20 percent coinsurance or copay.
Medicare coverage for nursing home care
If a patient has spent 3 days in the hospital, Medicare may pay for care in a Skilled Nursing Facility:
Days 1 – 20: $ zero co pay for each benefit period
Days 21 - 100: patient pays $185.50 coinsurance per day during 2021
Days 101 and beyond: patient pays all costs
Do you know your rights to nursing home coverage under Medicare? Medicare Part A pays for inpatient hospital care, and then for care in a skilled nursing facility IF the patient has a 'qualified' hospital stay of at least 3 days (not counting day of discharge) before being admitted to the skilled nursing facility.
What Is Medicare Copay For 2020
Medicare also pays for home health care, and the amount of reimbursement to home health care agencies also depends on whether the patient was admitted to a hospital before returning home. Patients who were put on Observation Status in the hospital end up paying out-of-pocket if they are discharged to a nursing home care:
Medicare is telling hospitals to keep patients 'under observation' to prevent eligibility for the 100 days of Skilled Nursing Facility benefits. A Medicare fact sheet warns patients to ask about their status when they are in the hospital: 'You’re an inpatient starting the day you’re formally admitted to the hospital with a doctor’s order. The day before you’re discharged is your last inpatient day.'Congress voted to require hospitals to tell Medicare patients when they are under observation care and have not been admitted to the hospital. The NOTICE law requires hospitals to provide written notification to patients 24 hours after receiving observation care, explaining that they have not been admitted to the hospital, the reasons why. The Notice must also disclose the financial implications for cost-sharing in the hospital and the patient's subsequent “eligibility for coverage” in a skilled nursing facility (SNF). Adobe music.
Medicare Part A Copay 2020 Dates
Medicare Advantage Discussion, Differences between Traditional Medicare and Medicare Advantage, 1 Page Factsheet, Caution on Medicare Advantage Plans
In a February 2, 2017 decision, the federal judge overseeing the Medicare 'Improvement Standard' case (Jimmo v. Burwell) ordered the Secretary of Health & Human Services to make it possible for nursing homes to comply with the Settlement, so discharged hospital patients can get rehabilitation. Many years after the Settlement was approved, the Center for Medicare Advocacy based in Willimantic, CT still hears from people who have been denied Medicare payment for home health, skilled nursing facility, and outpatient therapy. They advise Medicare beneficiaries and their families to continue citing the Jimmo Settlement materials linked on this page to challenge denials based on the old and erroneous “Improvement Standard.” Template Letter for Improvement Standard Appeal
If you go to the nursing home following a hospital stay, nursing homes are often reluctant to keep billing Medicare, because they think Medicare coverage depends on the beneficiary’s restoration potential; but the standard is whether skilled care is required:
Summary. Fact Sheet from Center for Medicare Advocacy. Even if full recovery or medical improvement is not possible, a patient may need skilled services to prevent further deterioration or preserve current capabilities. The nursing home patient who needs these skilled services should still be covered by Medicare.
FET Compression. What is FET Compression? FET (or Field Effect Transistor) compression came. Whats fet. What does FET mean? Field-effect transistor, FET (noun) a transistor in which most current flows in a channel whose effective resistance can be controlled by a transverse electric field. FET is an acronym for federal excise tax. It refers to the tax imposed by the federal government on tires used on the road with a maximum load capacity greater then 3500 pounds. Generally this applies to medium truck tires and heavy duty trailer tires. Credit for Fuel Used in Foreign Trade: An Overlooked Credit March 27, 2001. Most commercial operators avail themselves of the federal excise tax (FET) exemption for fuel contained in IRC section 4092, however many operators with international operations are not aware of. Federal Excise Tax on Trucks, Truck Bodies and Trailers The Federal imposes excise taxes on a variety commodities and services. Retail sellers of commercial and vocational vehicles, some truck and truck bodies, trailer and semitrailer bodies and chassis and truck tractors are subject to one of these federal.

The February 16, 2017 statement by Centers for Medicare & Medicaid Services (CMS) says: 'Skilled nursing services would be covered where such skilled nursing services are necessary to maintain the patient's current condition or prevent or slow further deterioration so long as the beneficiary requires skilled care for the services to be safely and effectively provided.'
'Skilled therapy services are covered when an individualized assessment of the patient's clinical condition demonstrates that the specialized judgment, knowledge, and skills of a qualified therapist ('skilled care') are necessary for the performance of a safe and effective maintenance program. Such a maintenance program to maintain the patient's current condition or to prevent or slow further deterioration is covered so long as the beneficiary requires skilled care for the safe and effective performance of the program.'
Hospital Observation Status can be financially devastating. Read More by Attorney John L. Roberts at: Agingcare.com 'This happened to us last year. After 4 days we were told the status was changing to outpatient.' More in Reader Comments.
Medicare Part A Copay 2020 Application
Getting Medicare to pay for skilled nursing home care.
Next Page: Medication Management: Preventing Polypharmacy, Maximizing Medicare Part D, and Finding Alternative Payment Sources
